AI Revolutionizes Early Disease Detection: Your Guide to Personalized Health
Introduction
For generations, healthcare has largely followed a reactive script: we feel sick, we see a doctor, we get a diagnosis, and then we begin treatment. This model has saved countless lives, but it often means we’re fighting diseases that have already taken hold. What if we could flip the script? What if we could predict and prevent illnesses before the first symptoms ever appear?
This isn’t science fiction. This is the reality being built today, powered by one of the most transformative technologies of our time: Artificial Intelligence. The AI revolution in medicine is here, shifting the focus from treating sickness to cultivating lifelong wellness. Through AI early disease detection, we can identify threats at their most nascent stages, while Personalized treatment plans AI can tailor therapies to our unique genetic makeup and lifestyle.
This guide will take you on a journey through the new landscape of preventative health AI. We’ll explore the groundbreaking AI in healthcare innovations that are making medical AI diagnostics more accurate than ever before. From analyzing medical images with superhuman precision to managing chronic conditions proactively, you’ll discover how smart healthcare solutions are creating a future where healthcare is predictive, participatory, and profoundly personal.
The Dawn of a New Era: From Reactive to Proactive Healthcare
The traditional healthcare model is based on intervention. It’s a system designed to fix problems after they arise. While effective, it’s like waiting for a warning light on your car’s dashboard to flash before you check the engine. AI for proactive health is the equivalent of having a master mechanic constantly monitoring every component, predicting potential failures, and recommending preventative maintenance.
This new paradigm is fueled by AI health data analytics. AI algorithms can process unimaginable volumes of data—from electronic health records (EHRs), genomic sequences, medical imaging, and even real-time data from wearables—to identify subtle patterns and correlations that are invisible to humans.
This shift offers immense preventative care AI benefits, including:
- Earlier Intervention: Catching diseases like cancer or heart conditions at Stage 0 or 1, when they are most treatable.
- Improved Outcomes: Proactive management leads to better long-term health and a higher quality of life.
- Reduced Costs: Preventing a chronic disease is far less expensive for both individuals and the healthcare system than managing it for a lifetime.
- Empowered Patients: Individuals gain deeper insights into their health risks and are empowered to make informed lifestyle choices.
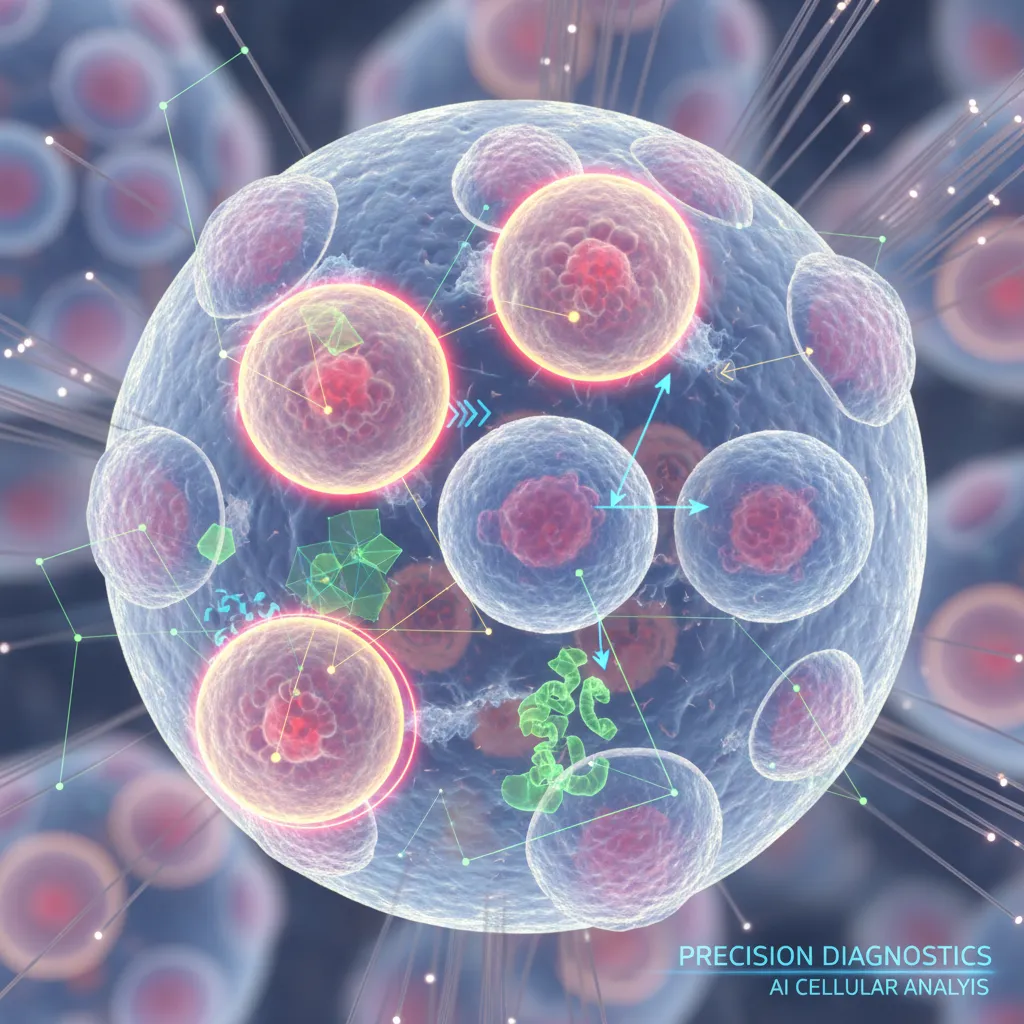
How AI Achieves Superhuman Accuracy in Early Diagnostics
At the heart of this revolution is the ability of AI to see what we can’t. By training on millions of data points, AI models develop an intuition for diagnostics that can augment, and in some cases surpass, human capabilities. This is where AI driven diagnostics truly shines.

Medical Imaging Analysis on Autopilot
One of the most mature applications of AI in healthcare is in medical imaging. Radiologists and pathologists spend their careers training their eyes to spot anomalies in X-rays, CT scans, MRIs, and tissue slides. It’s a skill that requires immense concentration and experience.
AI medical imaging analysis acts as a tireless, incredibly precise second pair of eyes. For instance:
- Early Cancer Detection AI: Deep learning algorithms can scan a mammogram and flag suspicious microcalcifications, a potential early sign of breast cancer, that might be missed by the human eye. Studies have shown AI can improve detection rates and reduce false positives.
- Neurology: In brain scans, AI can identify the subtle signs of a stroke or the early stages of Alzheimer’s disease by detecting changes in brain volume or structure long before clinical symptoms become obvious.
- Ophthalmology: AI can analyze retinal scans to detect diabetic retinopathy, a leading cause of blindness, allowing for timely intervention.
These tools don’t replace radiologists; they empower them. They handle the high-volume, pattern-recognition tasks, freeing up human experts to focus on complex cases and patient interaction, a prime example of AI in clinical decision support.
Predictive Analytics: Seeing Disease Before It Starts
Imagine your doctor telling you that you have an 85% chance of developing Type 2 diabetes in the next five years, giving you a precise roadmap of lifestyle changes to prevent it. This is the power of predictive AI in medicine.
AI models can analyze a patient’s entire health profile—EHRs, lab results, family history, and lifestyle data from apps—to calculate their risk for various conditions. This is a game-changer for AI chronic disease management:
- Heart Disease Prediction AI: Algorithms can assess hundreds of variables, from cholesterol levels to sleep patterns gathered from a smartwatch, to predict the risk of a heart attack or stroke with remarkable accuracy.
- AI Diabetes Risk Assessment: By identifying high-risk individuals early, healthcare providers can implement preventative programs focused on diet, exercise, and monitoring, potentially stopping the disease in its tracks.
- Sepsis Detection: In hospitals, AI constantly monitors patient vitals, alerting medical staff to the earliest signs of sepsis, a life-threatening condition, hours before a human clinician might notice.
Related: AI in Finance 2024: Top Tools and Trends You Need to Know
Decoding Our Blueprint: The Power of Genomic Medicine AI
Our DNA holds the secrets to our health. It can reveal predispositions to certain diseases and dictate how we’ll respond to specific medications. The challenge has always been the sheer complexity of the human genome.
Genomic medicine AI is the key to unlocking this complexity. AI algorithms can sift through billions of genetic data points to:
- Identify specific gene mutations linked to cancers, rare diseases, and inherited conditions.
- Predict a patient’s response to a particular drug, avoiding ineffective treatments and harmful side effects.
- Power the field of precision medicine AI, where treatments are no longer one-size-fits-all but are tailored to an individual’s unique genetic profile.
This granular level of insight is fundamental to creating truly personalized healthcare journeys.

Beyond Detection: AI-Crafted Personalized Treatment Plans
Identifying a disease early is only half the battle. The next step is determining the most effective course of action. This is where Personalized treatment plans AI come into play, representing one of the most significant AI patient care advancements.
From One-Size-Fits-All to Your-Size-Fits-One
Historically, treatments were developed for the “average” patient. But in reality, no such person exists. We all respond differently based on our genetics, environment, and lifestyle.
AI changes this by integrating vast datasets to create a holistic view of the patient. An AI system can analyze a patient’s tumor genetics, medical history, and data from millions of similar cases to recommend the most effective chemotherapy regimen with the fewest side effects. This is the essence of precision medicine AI in action, moving beyond broad-stroke treatments to hyper-personalized interventions.
Related: AI in Precision Health: Customizing Your Wellness Journey
AI in Clinical Decision Support: The Doctor’s Smart Co-Pilot
The goal of AI in medicine is not to replace clinicians but to augment their expertise. AI in clinical decision support systems act as intelligent assistants, providing real-time, evidence-based insights at the point of care.
Imagine a doctor consulting with a patient. An AI tool running in the background could:
- Scan the patient’s latest lab results and medical history.
- Cross-reference the information with the latest clinical trials and medical research.
- Flag potential drug interactions or suggest alternative diagnostic tests.
- Present a ranked list of potential diagnoses or treatment options based on statistical probability.
This empowers doctors to make faster, more informed decisions, backed by the collective knowledge of the entire medical field.
The Ecosystem of Smart Healthcare Solutions
The future of healthcare AI extends far beyond the hospital walls. It’s an interconnected ecosystem of digital health AI tools that integrate seamlessly into our daily lives, making health management continuous and intuitive.
Wearable AI and Continuous Health Monitoring
The smartwatch on your wrist or the fitness tracker on your belt is more than just a step counter; it’s a powerful health monitoring AI device. These gadgets collect a constant stream of data on heart rate, sleep quality, blood oxygen levels, and physical activity.
Wearable AI health monitoring platforms can analyze this data to:
- Detect irregularities like atrial fibrillation (AFib), a common heart arrhythmia.
- Monitor stress levels and promote mindfulness through biofeedback.
- Track the recovery of patients after surgery.
- Provide real-time data for managing chronic conditions like diabetes, creating a powerful feedback loop for AI personalized wellness.
Related: Apple Intelligence: Your Guide to a Smarter iOS 18 with AI
Revolutionizing Mental Health Diagnostics
Mental health is another frontier where AI is making a profound impact. Traditional diagnosis can be subjective and time-consuming. AI mental health diagnostics offer a more objective and scalable approach. AI models can analyze:
- Speech Patterns: Changes in tone, pitch, and pace can be early indicators of conditions like depression or Parkinson’s disease.
- Text Analysis: AI can analyze journal entries or text messages (with consent) to identify linguistic markers associated with anxiety or suicidal ideation.
- Behavioral Data: Patterns of smartphone usage can provide clues about social withdrawal or changes in sleep, key indicators of mental distress.
These tools can help identify individuals at risk sooner and connect them with the care they need, breaking down barriers to mental healthcare access.

The Road Ahead: Navigating the Future and Ethical Landscape
While the potential of AI in healthcare is immense, the path forward requires careful navigation. The implementation of these powerful technologies brings a host of challenges and ethical questions that must be addressed.
Overcoming Hurdles: Data Privacy, Bias, and Regulation
The most critical challenges revolve around AI healthcare ethical considerations:
- Data Privacy and Security: Health data is incredibly sensitive. We need robust regulations and security protocols to ensure that patient information used to train AI models is anonymized and protected from breaches.
- Algorithmic Bias: If an AI model is trained on data primarily from one demographic, its predictions may be less accurate for other groups. This could worsen existing health disparities. Ensuring datasets are diverse and representative is paramount.
- Accountability and Transparency: When an AI makes a diagnostic error, who is responsible? The developer? The hospital? The doctor? We need clear legal and ethical frameworks for accountability. Furthermore, “black box” algorithms, whose reasoning is opaque, must be replaced with explainable AI (XAI) so that doctors can understand and trust their recommendations.
- Regulatory Approval: Health technologies are rightly held to the highest standards. The FDA and other regulatory bodies are developing new frameworks to evaluate and approve AI-based medical devices and software to ensure they are safe and effective.
Related: What is GPT-4o? OpenAI’s New Multimodal AI Explained
The Future of Healthcare AI: What’s Next?
The AI health tech trends we see today are just the beginning. The future of healthcare AI promises even more integration and personalization. We can expect to see:
- Digital Twins: Ultra-personalized virtual models of individuals that can be used to simulate the effects of different treatments or lifestyle changes before applying them in real life.
- AI-Powered Drug Discovery: AI is already accelerating the process of developing new medicines by predicting how molecules will behave, drastically reducing the time and cost of research.
- Ambient Clinical Intelligence: AI systems that can listen to a doctor-patient conversation (with consent) and automatically document the visit, freeing the doctor from administrative tasks to focus entirely on the patient.
This is not just about revolutionizing medicine AI; it’s about fundamentally redefining our relationship with our own health.
Conclusion
We are standing at a pivotal moment in the history of medicine. The convergence of artificial intelligence, big data, and medical science is paving the way for a future that was once unimaginable. The era of reactive, one-size-fits-all healthcare is giving way to a proactive, personalized, and preventative model.
From AI powered health screening that catches diseases at their inception to precision medicine AI that tailors treatments to your unique DNA, these technologies are empowering both clinicians and patients like never before. While we must proceed with caution, thoughtfully addressing the ethical and regulatory challenges, the promise is undeniable.
The future of your health is not just about treating sickness when it arrives. It’s about building a personalized, data-driven roadmap to lifelong wellness, with AI serving as your trusted and intelligent guide on the journey.
Frequently Asked Questions (FAQs)
Q1. How is AI used for early disease detection?
AI is used for early disease detection primarily through two methods: analyzing medical images (like X-rays and MRIs) to spot subtle abnormalities the human eye might miss, and using predictive analytics. Predictive models analyze patient health records, genetic data, and lifestyle factors to calculate an individual’s risk for developing specific diseases like heart disease or diabetes long before symptoms appear.
Q2. What are the main benefits of using AI in healthcare?
The primary benefits include increased accuracy and speed in diagnostics, the ability to create highly personalized treatment plans based on an individual’s unique data, and a major shift towards preventative care. This leads to earlier intervention, better patient outcomes, and potentially lower healthcare costs by managing conditions proactively.
Q3. Can AI predict a person’s future health?
AI cannot predict the future with certainty, but it can predict risk with high accuracy. By analyzing vast datasets, predictive AI in medicine can identify individuals who have a high probability of developing a certain condition. This allows for targeted preventative measures to change that potential future.
Q4. What is an example of AI-driven diagnostics?
A classic example is in radiology. AI algorithms trained on millions of mammograms can screen for breast cancer by identifying suspicious patterns of microcalcifications. In many cases, these AI systems can detect signs of cancer earlier and with higher accuracy than human review alone, serving as a powerful tool for early cancer detection AI.
Q5. What are the ethical concerns surrounding AI in medicine?
The main AI healthcare ethical considerations include patient data privacy and security, the potential for algorithmic bias if training data is not diverse, a lack of transparency in how “black box” AIs make decisions, and determining accountability when an AI makes a mistake. Addressing these issues is crucial for the responsible adoption of AI in healthcare.
Q6. How does AI help create personalized treatment plans?
AI creates personalized treatment plans by integrating and analyzing a massive range of data specific to one person. This includes their genetic makeup (Genomic medicine AI), medical history, lifestyle habits, and even data from similar patients. The AI then suggests the most effective drugs, dosages, or therapies that are most likely to work for that specific individual, minimizing trial-and-error.
Q7. Will AI replace doctors?
No, the consensus is that AI will not replace doctors. Instead, it will augment their abilities. AI is a powerful tool for handling data analysis, pattern recognition, and administrative tasks. This frees up doctors to focus on what humans do best: complex problem-solving, patient communication, empathy, and making nuanced clinical judgments, using AI as an intelligent co-pilot.